What is heart health all about? Well, it’s a journey, the first steps in a journey of thousands. I’ve gone through some rather drastic lifestyle changes in recent weeks due to health issues. What I hope to do here is share some of my experiences and possible solutions. Perhaps one of you is going through a similar situation. Or, as I detail what happened to me, you may recognize similar issues with your own health or the health of someone you know. I am not a healthcare expert so I wouldn’t take anything I say as gospel. However, I will be working with doctors, dieticians, cardiologists, and other medical professionals. I will be relating, much of what they tell me in these pages. If some of what I have to say sounds familiar and relatable then you should consult your doctor for a professional opinion. My goal here is simply to inform and motivate. Hopefully something clicks with one of you. The life I save may be yours.
The first question is how did I arrive here? For many years now, I have been taking medication for hypertension. Just a few years back, my doctor noticed my cholesterol was creeping up and put me on medication for that as well. I’ve been a borderline diabetic for at least the last 20 years. During all of this, my doctor has told me that my best course of action is to lose the extra weight. I am, after all, packing on an extra 40 pounds or so. But anyone that is of a certain age knows that losing the weight is easier said than done. As we age, our metabolism slows down, we don’t exercise as much as we should, and let’s face it, we get into bad eating habits. After all, our generation was raised on McDonald’s.
My twisted logic through all of this was well, the doctor has me on medication for my hypertension and cholesterol so it’s under control. NOT! And I’m just a borderline diabetic. Never mind that it runs in the family. My grandfather on my father’s side was diabetic and my mom had it. My younger brother was recently diagnosed with diabetes. Also, my job as a machinist keeps me on my feet and walking around all day. It’s not exactly 2 hours at the gym, but I am getting exercise. And I felt reasonably healthy for my age. Sure, I had a lot of aches and pains, but I assumed that was just all a part of getting older. After all, I am 64 later this month. Bottom line, no matter how much I tried to rationalize and logic my way out of it, I was slowly poisoning myself to death. Even if I wasn’t going to listen to my doctor, my body was trying to warn me in subtle ways. It started with a nagging cough that I couldn’t shake, and it was getting worse. This is a result of fluid in my lungs and, left unchecked, it probably would have developed into pneumonia. It seems that I’ve been unusually tired lately and feeling very lethargic and run down. I would be sleepy at work and began taking 10-minute power naps at lunch time. After work I would go home and take a long nap. Again, I attributed this to not getting enough sleep at night, typically about 6 hours. And while that may have been partly true, there was more going on. Over the holidays I put on about 10 extra pounds, tipping the scales at close to 250. This is pretty common for me around the holidays and in past years I could easily drop 10 or 15 pounds quickly. Losing any more than that was the real challenge. But this time I couldn’t even drop the 10 or 15 pounds. I was thirsty and my mouth was always dry, a classic symptom of diabetes. I was getting up three and four times a night to pee. Some nights you could set a clock by my pee breaks every two hours. I further reasoned that this was related to my prostate (not uncommon in men of a certain age) and also contributed to my lack of sleep. In reality, it was another symptom of my diabetic condition. Occasionally I would have difficulty catching my breath. That was the one that actually put me in the hospital. I woke up on a Sunday morning and was unable to catch my breath. Simply walking the 20 or 30 feet from my bedroom to the attached garage and back left me winded. I decided it was time to see a doctor. And it was a good thing I did too. The takeaway from that little doctor visit was Number one, my blood pressure was elevated, so they had to adjust my medication. Number two, I have sleep apnea. Number 3, I am no longer prediabetic. I am now a full-blown diabetic. And Number 4, my heart had gone into arterial fibrillation.
So now I am, hopefully, on the road to recovery. But this means a whole new lifestyle. Junk food is gone. The two or three donuts on Friday mornings at work are a fond memory. An In ‘N Out double double animal style with animal fries and a chocolate shake are out of the question. Getting my weight back under 200 pounds is now a priority. I’ve cut most of the sodium out of my diet as well as carbohydrates. That means no more processed food. I’m reading labels and measuring portions. It’s really amazing the amount of salt in processed foods. I went through my refrigerator and gave away or threw out half of the food in it. A single serving of Boston frozen meatloaf dinner is 1680 milligrams of sodium. I’m trying to keep my sodium levels as close to 1500 milligrams as possible and that alone puts me over my daily limit.
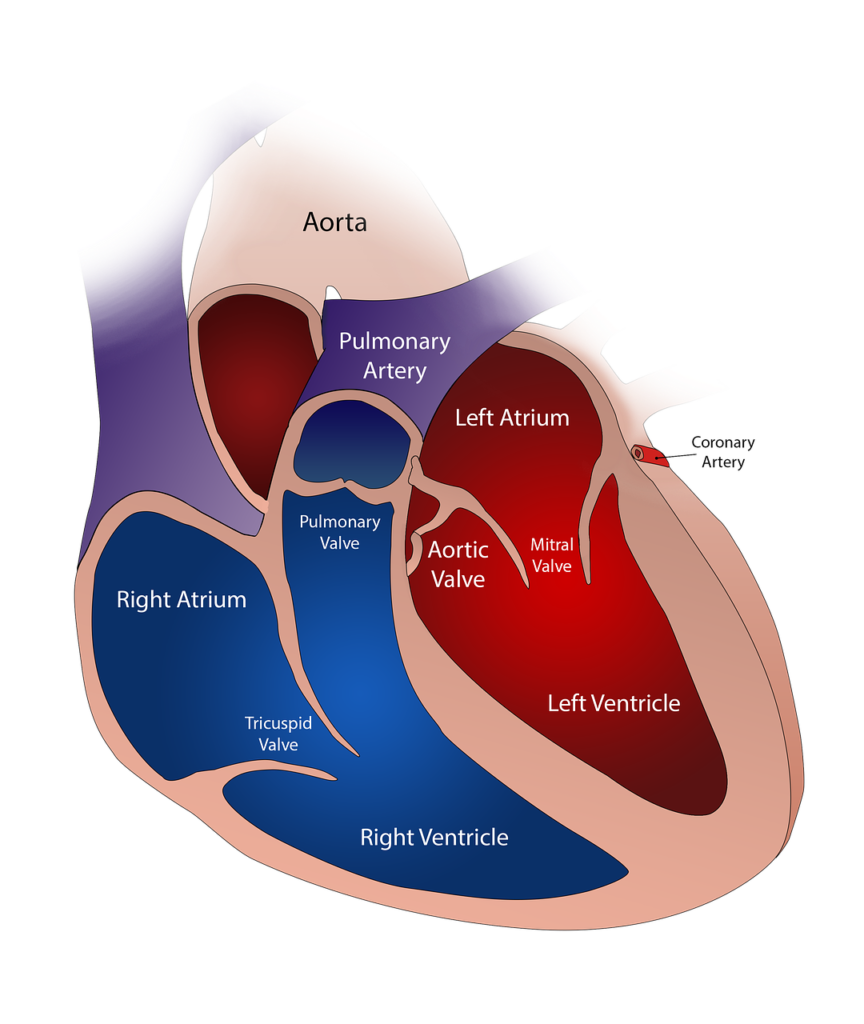
The first order of business, though, was to fix the problem with my heart. The typical heart has four chambers, two upper chambers, known as the atria, and two lower chambers known as the ventricles. Located in the upper right chamber of the heart, the right atrium, is a group of cells known as the sinus node. These cells act as a natural pacemaker for the heart by producing the signal that starts each heartbeat. This signal travels from the sinus node and through the two upper heart chambers. It passes along a pathway between the upper and lower chambers called the atrioventricular node. The movement of this signal along the atrioventricular node causes your heart to contract, or squeeze, forcing the blood into your arteries and thus to the rest of your body. Again, the normal heart will push out approximately 70% of the volume of blood it contains with each beat.
Arterial fibrillation, or a-fib, is defined as an irregular and rapid heart rate which commonly causes poor blood flow. The signals coming from the upper chambers of the heart are chaotic causing these chambers to shake or quiver. The atrioventricular node is then bombarded with signals trying to get through to the lower heart chambers. This causes the fast and irregular heart rhythm as described above. A normal heart rate is considered to be between 60 and 100 beats per minute. A person in a-fib will have a heart rate substantially higher than that. In my case, my resting heart rate was 180 beats per minute at one point, and only 35% to 40% of my blood was actually leaving my heart. This is because the chambers are opening and closing so rapidly not all of the blood can be evacuated. My cardiologist and new best friend, Dr. Micah Roberts, informed me, while this is obviously a concern, he had seen many cases where the flow was even less. While a-fib in and of itself is not usually fatal, the excess blood that is trapped in the heart tends to pool. When this happens, it can form clots. There is a strong possibility one of those clots might break off and go to the brain, causing a stroke.
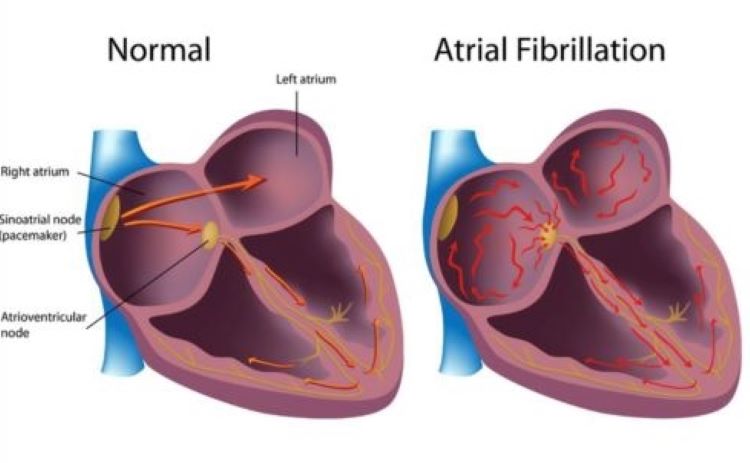
One of the scarier things about a-fib is that the symptoms can be very subtle, or they may not appear at all. Sometimes, a person goes into a fib and doesn’t even know it until they have a stroke. And then it’s too late. Symptoms of a-fib include,
- Heart palpitations, described as a sensation of a fast, fluttering, or pounding heartbeat.
- Chest pain.
- Dizziness.
- Fatigue.
- Lightheadedness.
- Reduced ability to exercise.
- Shortness of breath.
- General weakness.
Most of these symptoms can be written off as being caused by something else. You have a couple of days where you’re just extra tired, so you figure you need to get more sleep. You get a little lightheaded and you think maybe you just need to get something to eat. So, as I said, the symptoms can be very subtle. If they exist at all. There are different variations of a-fib as well. A-fib can be:
- Occasional, where the symptoms come and go. They may last for just a few minutes or possibly hours, although symptoms may persist for as long as a week. Episodes can happen repeatedly, and the individual will need to get treatment of some sort.
- Persistent, where the heart rhythm does not go back to normal of its own accord. A person with this type of a-fib may be treated with medications to restore and maintain normal heart rhythm.
- Longstanding persistent, where the a-fib is continuous and lasts longer than 12 months.
- Permanent, where the irregular heart rhythm cannot be restored. Medications, such as blood thinners, are needed to control the heart rate and prevent blood clots.
So, what exactly causes the signals in your heart to become so chaotic, triggering it to go into a-fib? Generally, problems with the structure of the heart are the most common cause. Some of the possible causes include:
- Coronary artery disease.
- Heart attack.
- A heart defect that you may have been born with.
- Problems with the heart valve.
- High blood pressure.
- Lung diseases.
- Physical stress due to surgery, pneumonia, or other illnesses.
- Previous heart surgery.
- Problems with the hearts’ natural pacemaker, the atrioventricular node.
- Sleep apnea.
- Various thyroid diseases.
- Use of stimulants including certain medications, caffeine, tobacco, and alcohol.
- Viral infections.
So, I was diagnosed with a-fib and my heart was beating a mile a minute. I had gone into the ER on Sunday, March 13, because I was having trouble catching my breath, and I was in the hospital until Wednesday afternoon. And that was just to get my heart rate under control with medication. I was still suffering from an irregular rapid heartbeat, but at least I wasn’t spiking at 180 beats per minute anymore. As stated before, one of the problems with a- fib is blood clotting and the chance of throwing a clot and causing a stroke. For that reason, Dr. Roberts put me on blood thinners for three weeks to reduce that risk. Once my blood was thinner and the chance of clotting greatly reduced, he could perform a procedure to fix the problem.
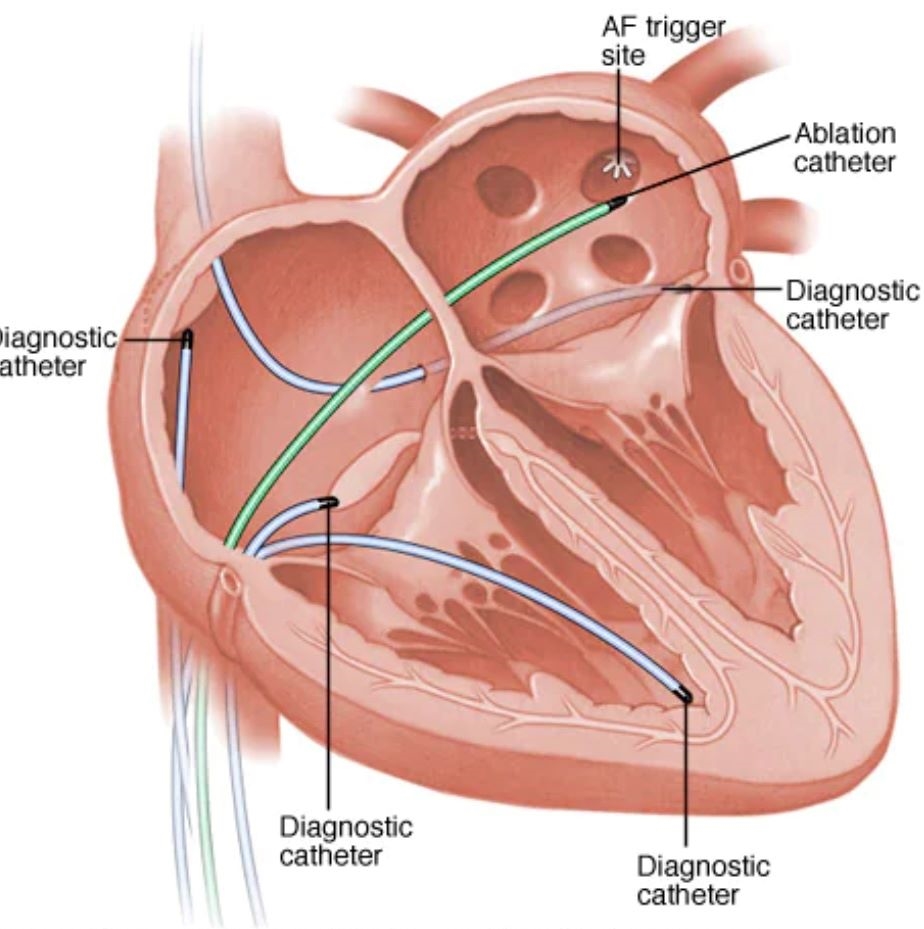
There are a couple of different ways to treat arterial fibrillation. One method uses an electric shock to jump start the heart back into a normal rhythm. The other method is known as cardiac ablation. Dr. Roberts felt the electric shock method was more of a short-term solution. Results vary with different individuals, but he felt the risk of my heart slipping back into a-fib were much higher using this method. Given my age, a young 64, and relatively good health, he felt that cardiac ablation was a better long-term method. The success rate is quite high, 90% after the first year. Although, with the passage of time, that rate comes down. After five years, it’s only 50%. The good news is, if my heart were to slip back into a-fib, I could always have another ablation. He said there was no limit on the number of ablation procedures, and I could have as many ablations as my wallet could withstand.
There are two methods for performing a cardiac ablation procedure. There is catheter ablation using radio frequency, or heat cauterization. Then there is catheter ablation using cryoablation, or freeze cauterization. In layman’s terms, they will fix the problem using either heat or cold. Dr. Roberts said he prefers the heat method over the cold, and, in fact, he knows of only one doctor currently using the cold method at Adventist Hospital, where I was being treated. He describes it as not unlike spot welding. He goes in through the groin with a catheter. In my case he went in on both sides. The catheter is just a long, thin plastic tube that goes in through the femoral artery on the way to the heart. Once he reaches it, he actually guides the catheter inside of the heart. Next, he inserts a thin wire through the catheter and into the heart. He locates the pulmonary veins, which is where the problem usually occurs as electrical signals here are misfiring and being sent to the ventricles. He then uses the wire to zap the misfiring cells around those veins. This kills the cells, isolating them from the rest of the heart and, even though the sinus node is still misfiring, the electrical impulses are localized. This allows the heart to drop into a normal rhythm. While he is in there, he said he would poke around to determine if there were any other areas where the signals are misfiring. A normal ablation procedure takes anywhere from 3 to 6 hours. He does so many of them he usually is on the lower end of that time estimate.
I checked into the hospital last Tuesday at 6:00 AM. After filling out the necessary paperwork I was escorted to a room where I changed into one of those backless hospital gowns. I was shaved so they could not only go in through my groin, but they also had to attach a series of electrodes to my chest so as to monitor the progress of the procedure. Around 10:00 AM I was wheeled into the OR where they transferred me to an operating table, hooked up an IV, and began attaching wires. Danny, my anesthesiologist, came in and we chatted a bit. I remember he injected something into my IV and the next thing I knew it was 1:30 and I was back in my room. I was still pretty groggy from the anesthesia, and it took the better part of the next hour before I was fully awake. My cardiologist stopped by to tell me everything went fine, and they would send me home with my wife around 3:30. After 24 hours I could remove the dressings and I was good to drive the next day. I should take a week off from work and avoid lifting more than ten pounds. I should also walk around because the movement was good for me. His office would call and schedule a follow up meeting in about three weeks but, if I had any concerns, I should call his office. Aside from my groin looking like Jake LaMotta used it for a speed bag, I felt pretty good. Getting up and down from bed or a chair was a bit difficult for a few days. I was also constipated and put on 8 pounds in two days, but Dr. Roberts said that was not unusual. Sure enough, it’s a week later and I’m the same weight as the day I went into the hospital, which is twenty pounds less than I weighed when I first went into the hospital on March 13.
There is more information I’d like to share so you can be aware of the health risks. You are at an increased risk of going into a-fib for the following reasons:
- Age. As far as I’m concerned, age is the root of all evil.
- Heart disease. This includes things such as heart valve problems, congenital heart disease, congestive heart failure, coronary artery disease, a history of heart attacks, or had previous heart surgery.
- High blood pressure. At least this one can be controlled with lifestyle changes and/or medication.
- Thyroid disease.
- Other chronic health conditions which can include diabetes, metabolic syndrome, chronic kidney disease, lung disease, or sleep apnea.
- Alcohol consumption. Especially binge drinking, but even casual drinking can trigger an episode.
- Obesity.
- Family history. The old tried and true standby.
Of course, as you age, the risk of stroke from a-fib increases. Especially if you have high blood pressure, diabetes, heart failure, or heart disease. I don’t know about you, but I was keeping score. In the previous lists, there are several things that keep popping up:
- Age is one. Hey, I’m 64 and I’m not living my life like Benjamin Button, so there’s not much I can do about that specifically.
- High blood pressure, which is something I have had for 20 years or more. And it runs in the family.
- Diabetes, of which I was only recently diagnosed, at the same time I went into a-fib.
- Sleep apnea of which I was also just recently diagnosed.
- Obesity and, as much as I hate that word, I have to be honest and look in the mirror. I don’t like what I see.
- Smoking, drinking, and caffeine consumption. Okay, I smoke cigars. But usually only one or two a week. But even that is too much now. In my so called ‘golden years’, I’m not a big drinker anymore. I enjoy splitting one or two bottles of wine with friends occasionally. And making trips to the wine country for wine tasting two or three times a year. Hard alcohol is maybe one or two drinks with dinner, when we go out. Which is only once or twice a month. Caffeine is probably my biggest problem. I drink a monster every morning. I also drink a lot of iced tea and, while I’m not a coffee drinker per-say, I do enjoy Starbucks Frappuccinos.
- Family history. Damn my ancestors.
Fortunately, I can do something about most of the above. The most important thing I can do is lose the weight. To do that I have to change my diet and lifestyle. Once I drop the weight, I need to keep it off by maintaining the diet and getting plenty of exercise. Losing the weight and keeping it off will have other benefits as well. It should reduce my high blood pressure. And I’m only type 2 diabetes and taking a pill for it. My doctor has told me I can get off the medication if I get my weight and blood levels under control. Now I just need a time machine so I can go back and beat some sense into my ancestors.
I went into the hospital on March 13. As I write this it is April 12. It has been an interesting month to say the least. I’ve dropped 20 pounds and counting. I purchased a Fitnus wristwatch that counts my steps and tracks my temperature, heart rate, blood pressure, oxygen levels and, as an additional feature, it tells time. I track my daily food intake, limiting sodium to 2000 mg or less, carbs to 200 or less, and calories to 2000 or less. I’ve cut caffeine and alcohol out of my diet as well as giving up cigars. The only red meat I’ve had in the last month is a 6 oz filet mignon when I attended the WonderCon. I’ve begun walking a half mile, around the block, each evening after work. I’ll probably start going to the gym next month when I’m fully recovered from my procedure.
That’s what this section is about. I plan to live to 100. Well, I’ve got 36 years to go and I need to start taking better care of myself. Hopefully I’ll inspire someone out there. I hope you will join me. In future blogs I’ll talk about dealing with diabetes and other health issues that we baby boomers all have to deal with, using my experiences as an example of what not to do and, hopefully, what you can do before it is too late. I’ll be sharing diet and exercise tips as well as healthy recipes. And, as always, I’ll be swinging for the fences all the way.
